Is RF Ablation Safer than Chemical Facet Neurolysis?
Author
Dr. Stephen Cosentino
PRESIDENT OF EMPIRE MEDICAL TRAINING Comparing Paravertebral Facet Joint Nerve Destruction Methods
Comparing Paravertebral Facet Joint Nerve Destruction Methods
There have been conflicting studies, interpretation, and a bureaucratic bias in relation to the various procedures used in the paravertebral facet joint nerve destruction associated with interventional pain management procedures. The debate has escalated recently as Aetna Insurance no longer will reimburse physicians for facet chemodenervation/chemical facet neurolysis. Medicare and other private insurance companies continue to reimburse for chemical facet neurolysis as the efficacy has been proven for (76) years and the benefits to the patient last (6) months to (1) year or longer and in some cases can be permanent.
It is the opinion of this writer that Aetna Insurance overreacted and the reality of their decision further alienates other medical specialties from practicing these medically necessary interventional pain management procedures as well as limiting the patient’s ability to receive these procedures. The point here is that patients generally need to be sedated for the RFA procedures (which most physicians do not want) and typically the cost of investment for such RF technologies is $40k - $50k thus limiting the number of physicians offering this procedure as well as the patients that can receive these procedures.
Chemical facet neurolysis has been used safely since 1936 and though there are complications that may occur with these injections the rate of complication is no greater than radiofrequency ablation (RFA) facet denervation procedures.
The (2) types of neurolytic agents most commonly used are phenol and ethyl alcohol with phenol (2-3%) being preferred. The destructive action of phenol involves inducing protein precipitation through the separation of the myelin sheath, axonal edema and the reduction of various cellular elements. Phenol also has an anesthetic effect as it temporarily blocks smaller nerve fibers and destroys small vessels and spares large fibers. The subsequent fibrosis that occurs makes nerve regeneration more difficult and/or impossible. The results are clinically evident after 5 to 7 days though the anesthetic effect lasts only 1-2 days. Phenol can be injected intrathecally and epidurally and can be used for peripheral, sympathetic, and para-vertebral somatic blocks.
Radiofrequency ablation (RFA) involves the placement of an electrode that produces heat (up to 60 degrees Celsius) by radio waves in order to destroy the sympathetic nerve supply. The patient needs to be sedated and the needle is placed under the skin in the direction of the median branch of the dorsal ganglion within the facet joint – image guidance must be used during the procedure. The destructive action allows for disruption of the unmyelinated nerve fibers (not permanent) and leaving the larger myelinated fibers unaffected.
The most common complication associated with both chemical facet neurolysis and radiofrequency ablation (RFA) is neuritis and post-lesioning neuritis which can be up to 10% of your patients. With chemical facet neurolysis, neuritis can only occur if the nerve cell body is not destroyed effectively. Another complication associated with both chemical facet neurolysis and radiofrequency ablation (RFA) is Anesthesia Dolorosa (numbness) which can at least be avoided with chemical neurolysis by performing a neurolytic block prior – this is not a common complication with either procedure.
Other complications for both procedures which are infrequent and temporary include possible skin or non-target necrosis of tissue (ischemia) and motor paralysis associated with either procedure. Chemical facet neurolysis also may lead to temporary bowel and bladder dysfunction though very rare and short duration (1-4 weeks respectively). Since chemical facet neurolysis involves the introduction of phenol there could also be systemic toxic reactions such as heart rhythm and blood pressure changes though extremely rare. Radiofrequency ablation also has other side effects including pneumothorax (collapsed lung), incomplete pain relief, and possible Horner’s syndrome in rare circumstances.
 The bottom line is that neither method for paravertebral facet joint nerve destruction is better or safer than the other. The major advantage to chemical neurolysis for patients is that the indication of pain can be relieved in less time (approx 1 month) rather than with RFA which will require additional therapeutic steroid injections that can delay relief for months where patients lifestyle issues are affected. Patients are also more unlikely to return to your practice after the steroidal injections wear off and tend to seek a pharmaceutical solution or surgical solution for their pain of which either solution is unacceptable.
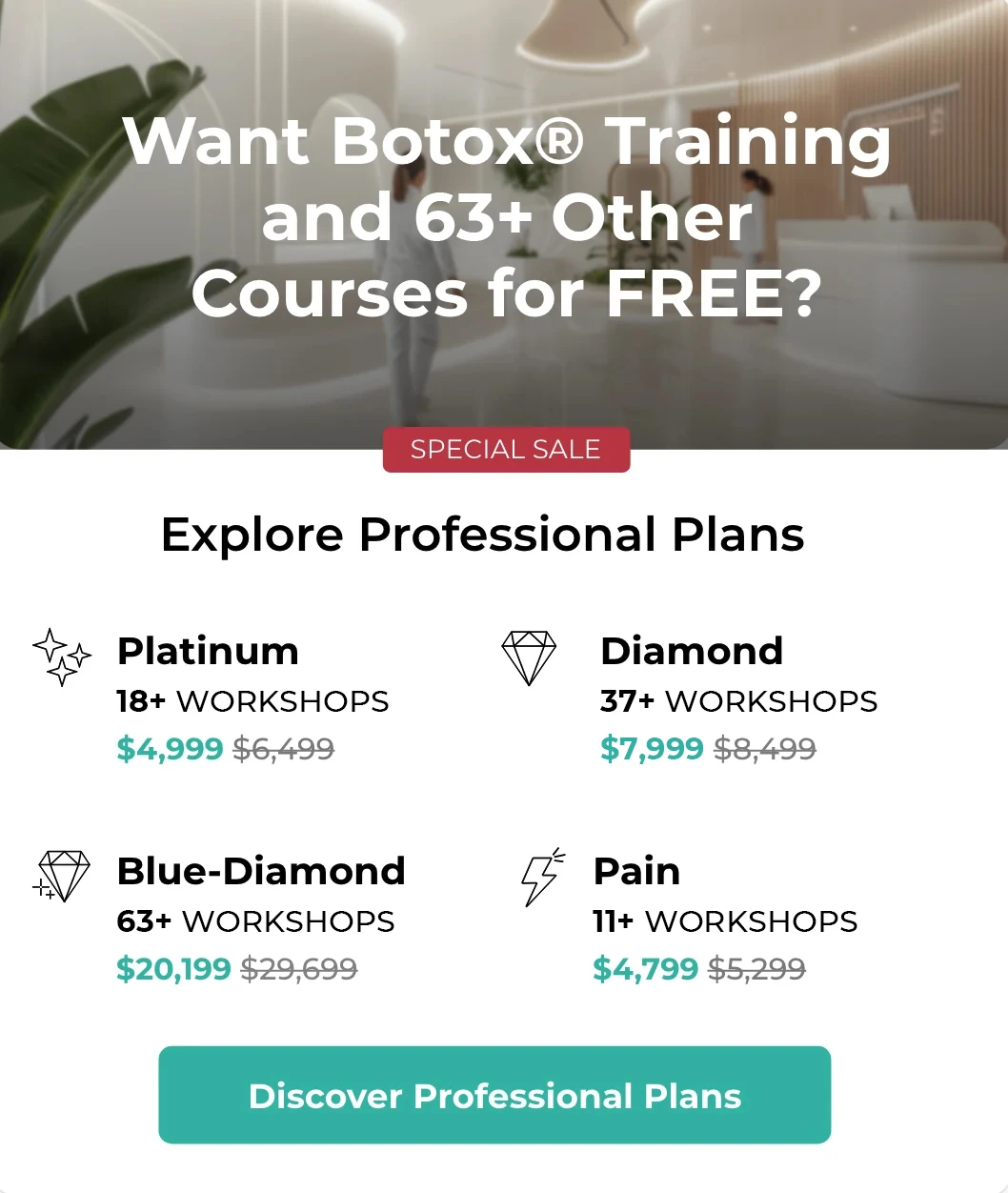
Empire Medical Training teaches both chemical facet neurolysis (3-Day Pain Show) and radiofrequency ablation (3-Day Pain Show) within our course study. RFA is featured within the as an alternative to chemical facet neurolysis as it may be impractical for many physicians to incorporate or integrate within their practice due to facility and capital requirements. Though we cannot necessarily recommend either method for paravertebral facet joint denervation over the other they are comparable in almost every manner of efficacy and possible complications associated with the procedure.
The bottom line is that neither method for paravertebral facet joint nerve destruction is better or safer than the other. The major advantage to chemical neurolysis for patients is that the indication of pain can be relieved in less time (approx 1 month) rather than with RFA which will require additional therapeutic steroid injections that can delay relief for months where patients lifestyle issues are affected. Patients are also more unlikely to return to your practice after the steroidal injections wear off and tend to seek a pharmaceutical solution or surgical solution for their pain of which either solution is unacceptable.
Empire Medical Training teaches both chemical facet neurolysis (3-Day Pain Show) and radiofrequency ablation (3-Day Pain Show) within our course study. RFA is featured within the as an alternative to chemical facet neurolysis as it may be impractical for many physicians to incorporate or integrate within their practice due to facility and capital requirements. Though we cannot necessarily recommend either method for paravertebral facet joint denervation over the other they are comparable in almost every manner of efficacy and possible complications associated with the procedure.